Integrating Electronic Health Records (EHRs) has been pivotal in modernizing healthcare. Transitioning from paper-based systems, EHRs have greatly improved data accessibility and patient care. As of 2021, nearly 4 in 5 office-based physicians (78%) and almost all non-federal acute care hospitals (96%) in the United States had adopted a certified EHR. It represents a significant increase from 2011 when 28% of hospitals and 34% of physicians had adopted an EHR. Generative Artificial Intelligence (AI) presents an opportunity to enhance these systems further. Generative AI, particularly models like GPT-4, introduces advanced cognitive functions to EHRs, going beyond traditional data analysis to generate insights and predictions, thus aiding clinical decision-making.
Generative AI integrates into the EHR system's architecture as an advanced analytics layer. This layer interfaces with the core EHR database, accessing patient data while ensuring privacy and security standards compliance.
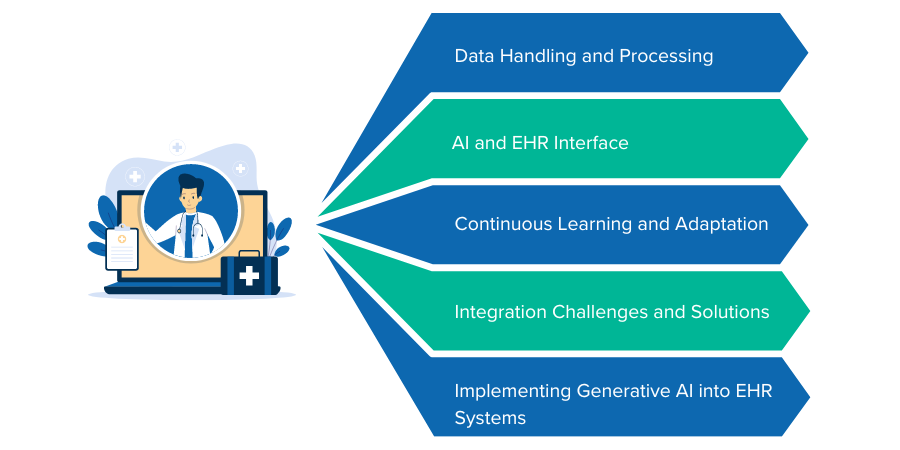
Data Handling and Processing: The AI processes health data using machine learning algorithms trained on vast datasets to identify patterns and make predictions. This process respects patient privacy by using de-identified data where possible and encrypting sensitive information.
AI and EHR Interface: The AI interface with EHR systems involves RESTful APIs and HL7 FHIR standards to ensure seamless data exchange and interoperability. The system design minimizes disruptions to existing workflows and is optimized for scalable and efficient data processing.
Continuous Learning and Adaptation: The AI models deployed within the EHR systems are designed for continuous learning. They evolve through ongoing exposure to new patient data and emerging medical research. Advanced algorithms, such as neural networks, facilitate this adaptive learning, regularly updated to maintain accuracy and relevance in clinical decision support.
Integration Challenges and Solutions: Integrating generative AI into existing EHR systems often encounter challenges such as data heterogeneity and system compatibility. Innovative solutions like middleware platforms for data normalization and advanced data mapping techniques have been developed to address these. Additionally, user-friendly interfaces are designed to ensure seamless interaction between healthcare professionals and the AI system, enhancing user adoption and minimizing training requirements.
Implementing generative AI into EHR systems is a complex process that requires careful planning and execution. The following key strategies are essential in guiding this complex integration.
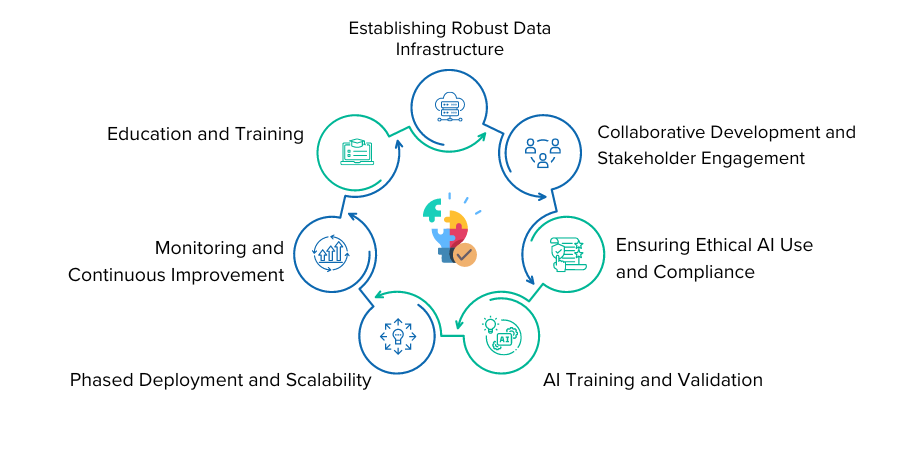
The cornerstone of effective AI integration is establishing a robust data infrastructure. It involves ensuring high-quality, consistent data as the foundation. It's vital to standardize data formats and guarantee the accuracy and completeness of health records.
Additionally, interoperability plays a crucial role in this process. The seamless exchange of data between different EHR systems and health databases is essential for the functionality of generative AI. Adopting FHIR (Fast Healthcare Interoperability Resources) standards can significantly enhance this interoperability.
A collaborative approach to development and stakeholder engagement is another critical strategy. It involves forming cross-functional teams comprising healthcare professionals, IT experts, data scientists, and ethicists. Their expertise ensures that the system meets clinical needs and meets ethical standards. Equally important is a user-centered design approach, where the AI interface and functionality are shaped by input from end-users like doctors and nurses, ensuring that the system aligns well with their workflows.
Ensuring ethical AI use and compliance is fundamental. It involves implementing advanced security measures to safeguard patient data, in line with regulations such as HIPAA in the USA and GDPR in Europe. Furthermore, developing and adhering to ethical AI frameworks is essential to ensure that AI decisions are explainable, fair, and free from biases.
Training and validation of AI are pivotal. Utilizing a diverse range of data sources for AI training ensures that it can handle a variety of clinical scenarios and patient demographics. Continuous validation is crucial, where the AI's performance is regularly tested and validated to ensure its accuracy and reliability, especially in clinical decision-making contexts.
Phased deployment and scalability are practical approaches to integration. Starting with pilot programs in specific departments or for certain functions allows for assessing performance and gathering feedback. Developing a scalable model ensures that AI can be expanded across different departments and healthcare settings.
Monitoring and continuous improvement are ongoing processes. Establishing metrics to evaluate the AI's impact on clinical outcomes, efficiency, and user satisfaction is vital. Additionally, creating mechanisms for continuous feedback from users helps identify areas for improvement and informs system updates.
Finally, education and training are indispensable. Providing comprehensive training for healthcare professionals ensures effective use of the AI-enhanced EHR system. Ongoing educational programs keep staff updated on new features and best practices.
Implementing generative AI in EHR systems represents a transformative step forward, potentially significantly improving patient outcomes and streamlining healthcare processes. By diligently following these strategies, healthcare organizations can effectively navigate the complexities of this integration, ensuring that the technology is used responsibly, effectively, and to its full potential.
Case Study 1 - Predictive Analytics in Chronic Disease Management: In a large European healthcare network, generative AI was integrated into EHR systems to enhance chronic disease management. The AI algorithms analyzed patient histories and lifestyle data to predict potential exacerbations in chronic conditions like diabetes and COPD. This intervention led to a 30% reduction in emergency hospitalizations and significantly improved patient self-management due to timely and personalized healthcare recommendations.
Case Study 2 - AI-Driven Personalized Treatment Plans in Oncology: A renowned cancer research center in the United States implemented generative AI to develop personalized oncology treatment plans. The AI system analyzed patient genetic profiles, historical treatment responses, and ongoing research data to suggest tailored treatment protocols. This approach increased the success rate of first-line treatments by 40% and considerably improved patient survival rates.
Case Study 3 - Enhancing Diagnostic Accuracy in Radiology: A multi-specialty hospital in Singapore introduced an AI module in its radiology department. The AI system, equipped with deep learning capabilities, analyzed thousands of radiographic images to assist in early and accurate diagnosis of lung nodules and breast cancer. The implementation reduced diagnostic errors by 20% and accelerated the reporting process, enhancing patient throughput and satisfaction.
As we conclude our exploration into integrating generative AI into Electronic Health Record systems, it's clear that we stand on the brink of a healthcare revolution. This technological integration is not merely an incremental advancement but a fundamental shift that promises to redefine every aspect of healthcare delivery.
It is imperative to maintain a balanced approach as we integrate generative AI into healthcare. While embracing the benefits of this technology, we must also remain vigilant to its limitations and potential pitfalls. The goal should always be to enhance human elements in healthcare rather than replace them.

 Batoi Corporate Office
Batoi Corporate Office